What is adenomyosis?
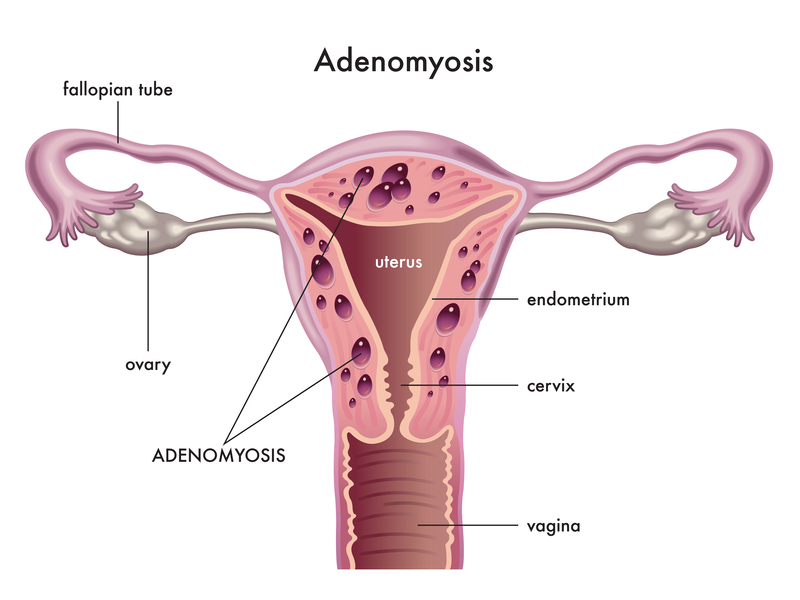
Adenomyosis is where the inner lining of the uterus invades the muscle wall of the uterus. It is similar to endometriosis which is where the inner lining of the uterus is found in other parts of the body, such as in the fallopian tubes or attached to the ovaries. Adenomyosis is where it buries into the muscle wall of the uterus.
The causes of adenomyosis are unclear. Three potential causes are postulated1:
- The lining cells are already present at birth within the uterine wall
- The lining cells grow into the muscle due to surgery
- The lining cells grow into the weakened muscle due to the birthing process
Oestrogen is required for adenomyosis to grow. So, the majority of women diagnosed with adenomyosis are in the reproductive age. It is thought that 10% of women of reproductive age who have had children and are aged between 40-55 years old have adenomyosis2. It goes away after menopause when oestrogen production drops.
What are the symptoms for adenomyosis?
In the early stages, patients do not have any symptoms at all. The possibility of adenomyosis is suggested incidentally on ultrasound. Eighty percent of people with adenomyosis have uterine fibroids and patients often present with symptoms related to the uterine fibroids2. When adenomyosis is more advanced, patients can present with1:
- Painful periods
- Heavy periods
- Bleeding between periods
- Painful intercourse (dyspareunia)
- Chronic pelvic pain
- Anaemia from the heavy periods
- Clinical examination by a doctor can find a tender and bulky uterus
How do you diagnose adenomyosis?
Adenomyosis is quite difficult to diagnose.
The clinical symptoms and examination findings are non-specific.
There is no blood test to diagnose adenomyosis.
Ultrasound or MRI can assist with diagnosis but requires specific expertise to detect subtle changes on imaging studies. A transvaginal ultrasound is often the first line investigation showing mottled appearance of the inner lining of the uterus, cystic spaces within the uterine wall and an enlarged, globular uterus2.
A biopsy of the tissue to confirm diagnosis requires anaesthetising the patient and can still be subjected to sampling error ie. if you take a sample from an area of the uterine wall that doesn’t have adenomyosis you could come to the incorrect diagnosis3.
Ultimately, definitive diagnosis of adenomyosis is made on hysterectomy where the uterine wall can be dissected to confirm the diagnosis. This is not ideal in many cases.
What treatments are available?
Management of the adenomyosis is determined by the severity of symptoms and the childbearing plans of the women.
- There are options to manage the symptoms of patients with oral medications1:
- reduce pain eg. non-steroidal anti-inflammatory drugs – mefenamic acid or naproxen
- reduce blood flow eg. tranexamic acid
- For women who need to retain the uterus, the more effective medical management options include2,4:
- Hormonal intrauterine device (IUD) insertion
- it causes thinning of the lining of the uterus reducing the heavy bleeds
- it does not affect the ovarian hormone production so does not stop the growth of the adenomyosis so the ongoing increase in the size of the uterine will further increase pain
- GnRH agonists
- these drugs are used to suppress normal ovarian hormone production and therefore starve the adenomyosis of fuel to grow
- patients will not experience periods as GnRH agonists induce menopause chemically and so reduce pain and bleeding
- some patients may not tolerate the side effects of menopause
- Hormonal intrauterine device (IUD) insertion
If the hormonal IUD or GnRH agonist is removed, the patient’s adenomyosis symptoms return. This means that the treatment is reversible and allows the woman to consider childbearing in the future.
- Uterine artery embolization is an invasive, non-surgical option. In this procedure, the uterine artery is occluded by injection of small particles via a catheter that is inserted from the groin. While symptoms may improve, pregnancy following this procedure has higher complications rates so this option is not recommended for women who are yet to have children2.
- Surgical options:
- Removal of localised adenomyosis (adenomyomas) is challenging surgery with a view of maintaining or perhaps improving fertility. The success rate of achieving pregnancy after removal of localised adenomyosis is only 60% if all the disease is removed, and is less than 60% if only partial disease is removed3.
- Endometrial ablation can be used to remove the inner lining of the uterus, thereby removing bleeding risk. Pregnancy is contraindicated after this procedure is performed.
- Hysterectomy, the complete removal of the uterus, is the gold standard of treatment for women who have completed or have no desire for childbearing2,3. It alleviates symptoms and removes the risk of recurrence by eliminating the disease by removing the organ. This is not an option for many women who still desire future fertility.
What is the impact on fertility?
Women in their 30s and 40s have less spontaneous pregnancies and less success with in-vitro fertilisation (IVF). The presence of adenomyosis can change the way the fallopian tubes and uterus contract leading to poor passage of sperm to allow for conception to occur and inhibits implantation of the embryo into the uterus3. Success rates with IVF are reported to be reduced to less than 50% due to a combination of factors3.
What is the impact on pregnancy3?
Adenomyosis can affect how the placenta grows, affecting the growth of the baby. It can lead to poorer growth of the baby, premature rupture of membranes, rupturing of uterine wall due to thinning and a greater risk of placental problems.
Adenomyosis is a complex condition with much more to be learnt about why it occurs and how to treat it. Please see your local doctor to discuss further about this condition if you have any questions or concerns.
References:
- Jean Hailes, 29 June 2021, Health topics, vulva vagina ovaries & uterus, adenomyosis, https://www.jeanhailes.org.au/health-a-z/vulva-vagina-ovaries-uterus/adenomyosis
- Sydney Care Centre for Advance Reproductive Endosurgery, 2021, patients, conditions, adenomyosis, https://www.sydneycare.com.au/patients/conditions/adenomyosis/
- Endometriosis Australia, 9 September 2020, Prof Jason Abbott; Adenomyosis – sister to endometriosis or distant cousin? https://www.endometriosisaustralia.org/post/2016/11/08/adenomyosis-sister-to-endometriosis-or-distant-cousin
- Sydney Fibroid Clinic, 2019, Adenomyosis treatment, https://www.sydneyfibroidclinic.com.au/adenomyosis/adenomyosis-treatment/











